
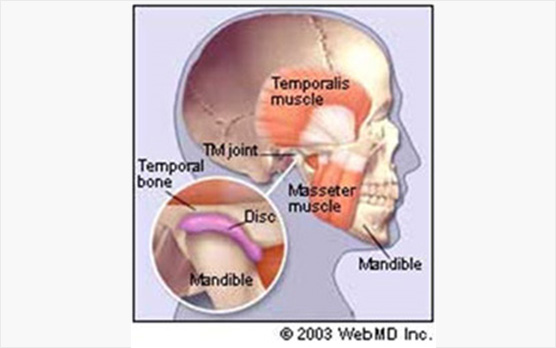
The temporomandibular joint is the joint that connects the lower jaw (mandible) to the skull, and is located immediately in front of the ear on each side of the head.
The joints are flexible, allowing up and down as well as side to side movements to be performed and enabling you to talk, chew, and yawn. Muscles attached to and surrounding the jaw joint and lower jaw control the position and movement of the jaw.
Temporomandibular disorders (TMD) occur as a result of problems associated with the jaw joint and surrounding facial muscles that control chewing and movement of the jaw. Injury to the jaw, temporomandibular joint, or muscles of the head and neck – such as from a heavy blow or whiplash – can cause TMD. Other possibilities include:
People with TMD can experience severe pain and discomfort that can be temporary or last for many years. More women than men experience TMD and TMD is seen most commonly in people between the ages of 20 and 40. Common symptoms of TMD include:
A careful patient history and clinical examination to exclude similar symptoms resulting from toothache, sinusitis, arthritis or gum disease will be done.
The surgeon will examine your temporomandibular joints and associated muscles for pain or tenderness; listen for clicking, popping or grating sounds during jaw movement; look for limited motion or locking of the jaw while opening or closing the mouth; and examine bite and facial muscle function. Sometimes panoramic X-rays will be taken. These full face X-rays allow your surgeon to view the entire jaws, TMJ, and teeth to make sure other problems aren't causing the symptoms. Sometimes other imaging tests, such as magnetic resonance imaging (MRI) or a computer tomography (CT), are needed. The MRI views the soft tissue such as the TMJ disc to see if it is in the proper position as the jaw moves. A CT scan helps view the bony detail of the joint.
Treatments range from simple self-care practices and conservative treatments to injections and surgery. Treatment should begin with conservative, nonsurgical therapies first, with surgery left as the last resort. Surgery does not guarantee resolution of symptoms.
BASIC TREATMENTS
OTHER TREATMENTS
When the basic treatments listed above prove unsuccessful, your dentist may suggest one or more of the following:
Compared with arthroscopy, open-joint surgery results in a longer healing time and there is a greater chance of scarring and nerve injury.